Shining a light on Hidradenitis Suppurativa (HS)
A rarely heard, barely discussed, and seldom treated chronic skin condition that deserves a blog of its own.
Hidradenitis Suppurativa (HS)
Commonly known as Acne Inversa, Hidradenitis suppurativa (HS), is a chronic inflammatory skin condition that affects areas experiencing the most contact, the apocrine gland-bearing skin in the axillae, groin, and under the breasts.
Clinically characterized by:
Open double-headed comedones
Painful firm papules and nodules
Pustules, fluctuant pseudocysts, and abscesses
Draining sinuses linking inflammatory lesions
Hypertrophic and atrophic scars.
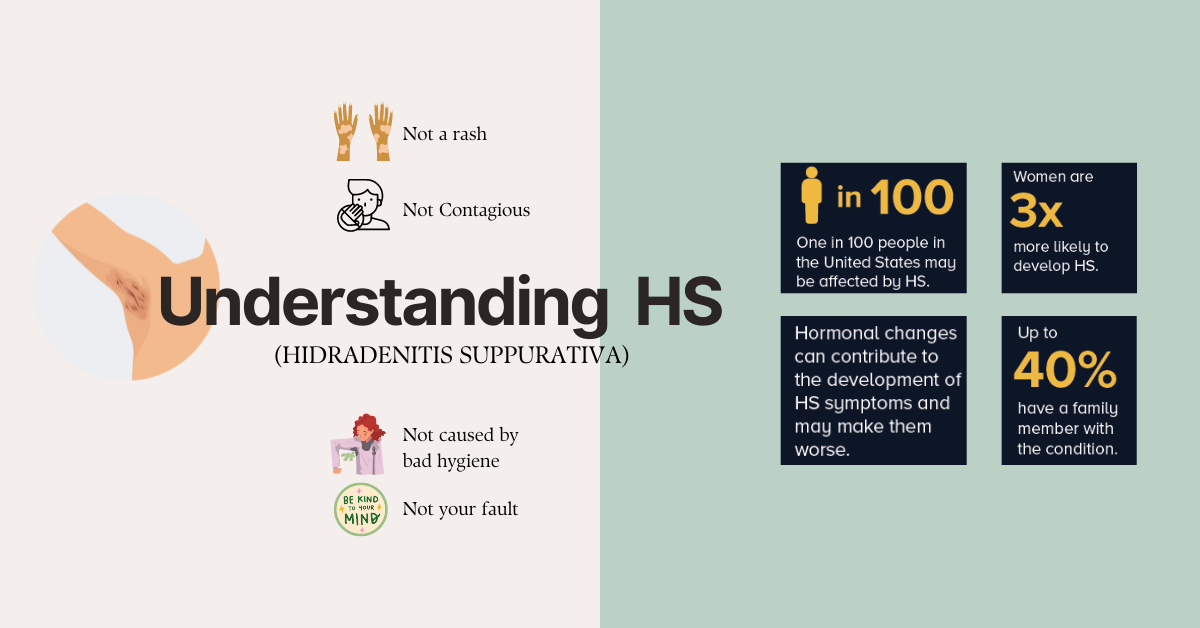
People are often unable to diagnose this condition, sometimes it takes much longer to diagnose and even longer to treat. This leads to severe depression and trauma in most. More than anything, HS can be painful, with open wounds that may leak blood or pus and be uncomfortable when they rub up against the skin or clothing. What’s important is to acknowledge and create awareness that,
Hidradenitis suppurativa is:
● NOT a sexually transmitted disease
● NOT caused by unclean skin
● NOT contagious
● NOT acne
Understanding how HS may progress for each individual, might help treat and support the people going through it.
Who gets Hidradenitis Suppurativa & what causes it?
Hidradenitis suppurativa is thrice more common in women than men. If you are an African- American woman living in the United States, chances are that for every 100,000 African Americans, 296 have had HS (according to a study conducted in the year 2017). Acne Inversa takes its most active form between the ages of 20 and 40 years, and in women can resolve at menopause.
It’s not your fault. It can happen to almost anyone. It may run in the family. Factors thought to contribute to HS include one’s weight and smoking. HS is more common in women with polycystic ovary syndrome (PCOS), a condition that causes hormonal imbalances. Some women may also experience HS flares around the time of their menstrual period. A heavier weight means more skin contact and sweat glands. Similarly, smokers may be more prone to it.
The term ‘hidradenitis’ implies an inflammatory disease of the sweat glands. It has recently been discovered that HS is an autoinflammatory syndrome (ask more about this from your dermatologist).
Many people have never heard of Hidradenitis Suppurativa.
Dermatologists are trained to recognize HS.
While a patient may simply think of HS as having pimples, sores, or lumps on their armpits or groin, to a dermatologist’s trained eye, there are differences between HS and other conditions like acne and boils.
With an accurate diagnosis and proper treatment for HS, you can:
Prevent HS from worsening
Relieve pain
Improve wound healing
Treat an infection, which can develop if you have an open wound
Your dermatologist might work closely with other doctors to determine if you are at risk for developing health conditions like arthritis, diabetes, and/or heart disease.
If you have HS, the chances of risk are greater and your dermatologist might just prevent you from falling victim to any of these conditions. Having someone to talk to about it relieves half the toll this condition takes on your mental health.
We want to educate you about the signs and symptoms so you may help dermatologists like us provide you with a prognosis in the earliest phase. Your dermatologist can also watch for signs of skin cancer on your skin.
Caught early, Skin Cell Carcinoma (skin cancer) is highly treatable.
Can HS be CURED?
HS cannot be cured, but treatment can control the disease. Treatment can prevent new HS and treat existing HS. You continue to live your life on your terms but stay vary of exhilarating the condition.
How can I manage my symptoms?
People with HS are advised to wear loose-fitting clothing to help reduce sweat and keep moisture from causing further irritation and pain to HS bumps and open wounds. Quitting smoking and managing one’s weight may help with the symptoms of HS. Avoid using washcloths, loofahs, or any abrasive material, as they may irritate the skin. Do not squeeze bumps and sores. Avoid shaving or using hair-removal creams.
Keeping track of your signs and symptoms might be the thing that helps you most in your journey of treating HS. Keep one handy journal to keep notes of your symptoms and diagnosis the next time you visit your dermatologist.
Your strength and willingness are your best partner during this painful time. Pause and relax. You are not alone.